Let's take a look at how this all started, at least from the time that I became
 |
| Bruce G Larson after initial surgery |
suspicious something was not right.
It started with a lump in my jaw and I had pointed it out to my
family doctor last fall, but they decided it was something they can
just keep an eye on. As we inched into the new year, the lump had
grown larger and I was beginning to experience pain in my jaw and
under my tongue, especially when eating.
I went to the emergency room at a local hospital and their
determination was that I had a salivary gland stone that could likely
work itself out by using lemon drops. Two weeks later, the pain was
increasing, sometimes unbearable, so I returned to the emergency
room. They concluded, once again, that is was the salivary gland
stone but suggested I see a specialist if things don’t start
getting better.
A couple of weeks later, I saw a local ear, nose, throat
specialist and they referred me to an otolaryngologist. They
determined the growth had to be removed. They scheduled a surgical
procedure and ordered some further tests at the hospital. Initially,
the doctor was not overly concerned and said the surgical process,
with recovery, would take about 3 days.
However, when the fine needle biopsy results were reviewed by the
doctor, she called me to tell me the news. It was determined that I
had cancer and the surgery would be more extensive than originally
planned. Specifically, the cancer was termed malignant neoplasm,
floor of mouth, Stage III. Reconstruction of my mouth would be required.
The surgery took over 8 hours at Florida Hospital, Celebration on
March 11,
 |
| Florida Hospital, Celebration |
2014 and that was followed by 3 days in ICU and 4 more days
in a standard hospital room for observation.
I don’t recall much about what happened during the recovery
process in the hospital. A lot of the time was spent just trying to
figure things out. It was not clear what was next: the chemotherapy,
radiation, the healing. The way I was feeling, I had many more
questions than I did before. But I knew I had to somehow regain the
faith I would need to overcome this disease.
On March 17, I was released from the hospital and taken home by
ambulance.
I then spent a few weeks getting used to things at home. I have
the Percutaneous endoscopic gastrostomy (PEG) tube inserted in the
stomach for liquid nourishment and for taking medications.
A hospice
nurse came twice a week at first then once a week until the insurance
 |
| What was taken became part of my tongue |
company (not the doctors) released her. But she was able to show us
how to change dressings, how to properly use the peg tube and also
advised us of the medical supplies we would need. She also reviewed
proper use of the oxygen tanks, the suction machine and the
nebulizer.
There were problems sleeping too. I was not able to lay in my bed
comfortably because the neck and throat were swollen and when I would
lay flat, the air supply seemed to be limited. So I slept in a
recliner since I was able to adjust the angle of my throat by
positioning my back and head I was supposed to start chemotherapy and
radiation treatment about 4 weeks after surgery, but I had been given
an antibiotic for some reactions I was having in my mouth. These
evidently caused lower intestinal bleeding and I was taken by
ambulance back to the hospital.
While undergoing a series of tests,
it was discovered that had contracted C-Diff , but that was cleared
in a couple of days. I was, however, able to get a much needed
colonoscopy while anesthetized. Thankfully, just one benign polyp was
found and that was removed.
The following week, the radiation and chemotherapy had to start or
I would be falling behind in the recommended treatments. Certainly, I
had no idea what to expect, but I was prepared to lose my hair. I
even bought a baseball cap that said “Cancer Sucks,” (just in case, of course).
The cancer,
by that time, was upgraded to Stage IVa.
I was not able to sleep in my bed comfortably because the neck and
throat were swollen and when I would lay flat, the air supply seemed
to be limited. So I slept in a recliner since I was able to adjust
the angle of my throat by positioning my back and head.
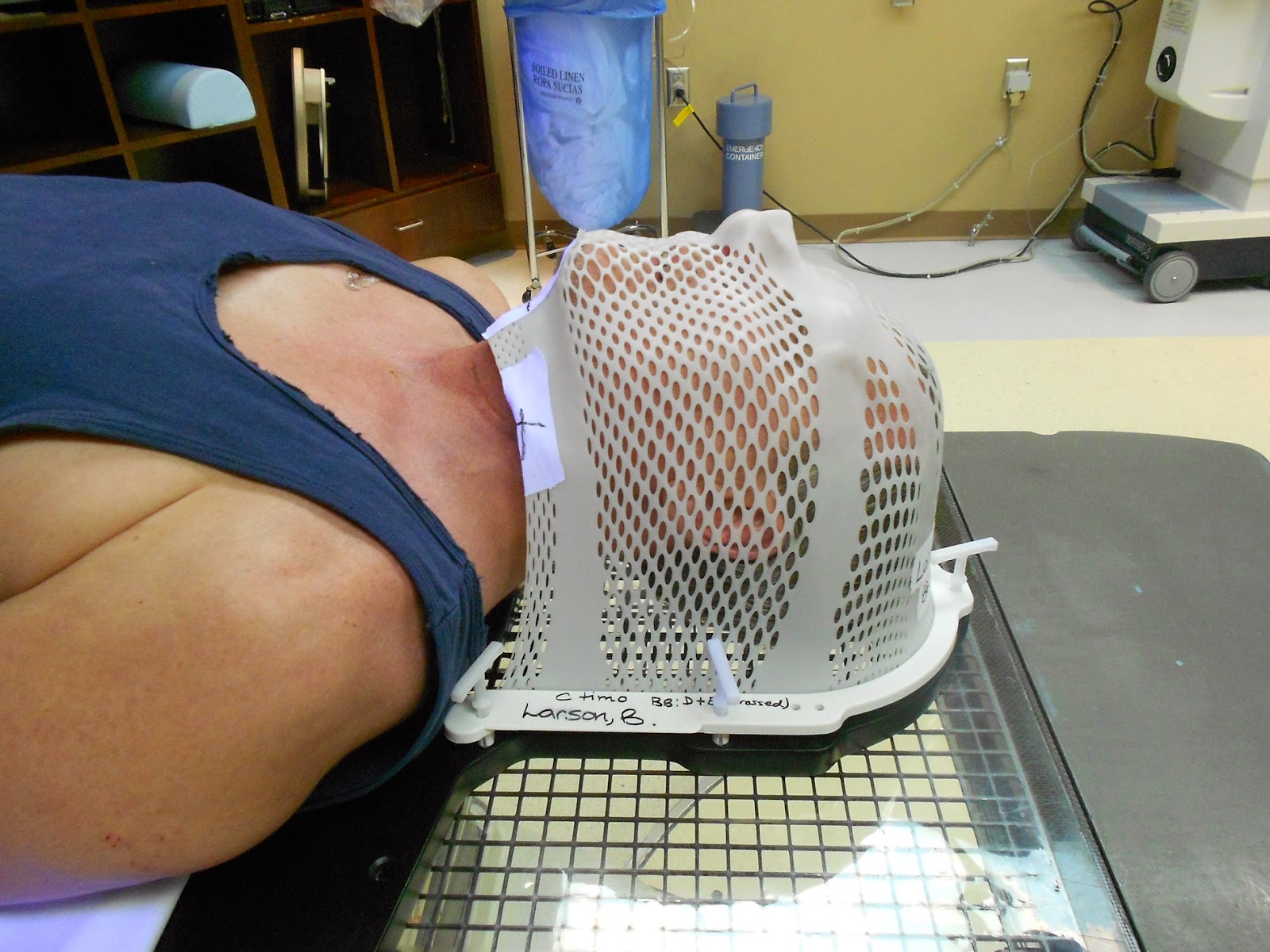
This issue almost caused another set-back to the treatment. The
radiation therapy staff asked me to lie down on a table so they could
fit the mask that I would have to wear for each treatment. They heat
the plastic mask then form it to the contours of my face.
This mask
would then be clamped to the treatment table to make sure once the
coordinates were established, I would not be able to move.
I explained that I was unable to breathe while laying on my back,
and the doctor
 |
| Bolted to the radiation therapy table |
|
in charge told me that I would be able to breathe. I
was frightened and was not sure what to do. I asked for a different
doctor since I was not comfortable with him. He, in my opinion, would
not work with me to solve this problem. I was assigned to the another
doctor in that department and after meeting him, I felt much better.
He provided me with a prescription for Xanax to help ease the
anxiety.
I spent an afternoon laying on my back in the living room,
extending the amount of time at comfortable intervals. Each radiation
treatment required that remain laying down on my back for about 20
minutes.
Later, I met with the oncology social worker and she took the time
to sit with me while the first Xanax dose was settling into my
system. She went over breathing techniques and what to do if it felt like
I could not breathe.
I can’t say that I fearlessly walked into the treatment room, but
the staff greeted me with re-assurances that I would be ok and that
if I felt something was going wrong, I needed to release the hand
grips that pull my shoulders into place. They would notice this
through the cameras in the treatment room and they would come to my
aid in a matter of seconds. Remember, I remained clamped to the table
and was not able to move. The table is also raised about 5 feet so
the radiation machine could reach any angle necessary.
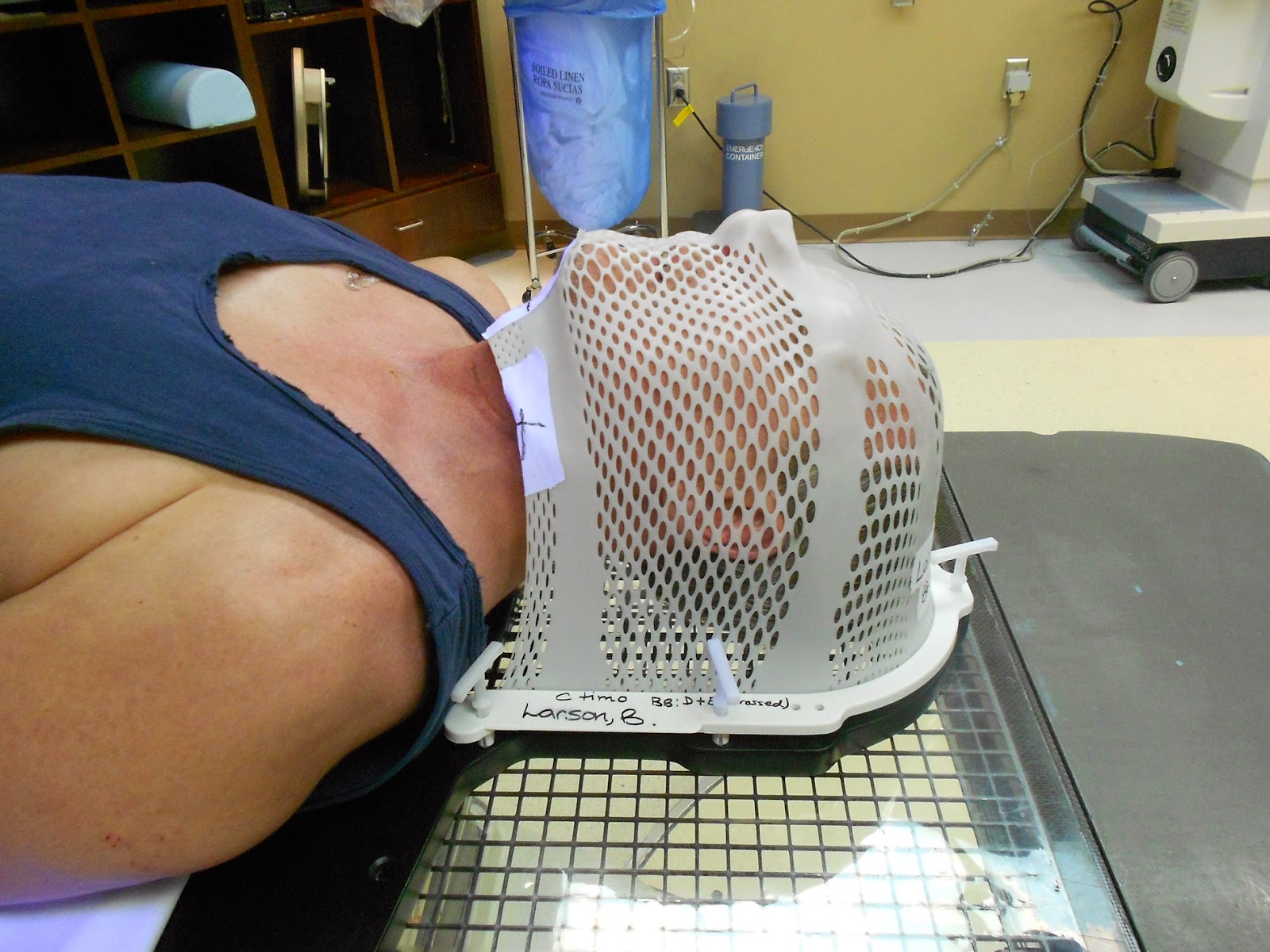 |
| I still have this mask as a "souvenir" |
My first complete radiation treatment took place on April 14
followed by my first day of chemotherapy on April 16. On April 17, I
had a Bard Power Port surgically implanted in my upper chest. This
allowed access for the chemotherapy treatments. The treatment plan
called for 37 radiation treatments consisting of 16 fields each day and
chemotherapy treatments once per week.
As the treatments continued, the process kept on getting easier
and easier. There were some days that were more difficult than
others. This was primarily due to an excessive mucus build-up that
occurs from radiation. I always learned, however, that I would still
be able to breathe despite this additional blockage. On May 22, I was
pleased to learn that the radiation fields were reduced from 16 to 6.
It’s odd, but these treatments became a part of me. They
provided a comfort zone. Maybe because so many things were going on,
so many changes in my body and in my emotions, I felt safe going to
the hospital. I would know what was going to happen, for the most
part. I felt like these doctors, nurses, technicians were all rooting
for me and I knew that they were – and still are.
After my initial shave 4 weeks following surgery (there were
sutures under my jaw from ear to ear), I hardly had to shave again.
The radiation did the shaving for me. I sometimes have to ask Vi now if I got all 7 remaining whiskers after I shave.
My final treatment, as I understood it, would fall somewhere
around June 14. I was looking forward to this last day and the
opportunity for me to ring the “Bell of Finality,” as some call
it. It is a bell that the patient rings on his or her last day of
radiation treatment. I had never seen it there at Florida Hospital,
Altamonte, but knew it had to be there somewhere. Perhaps in an area
further away from patients to keep from startling them.
 |
| Celebrating the final radiation treatment |
|
|
But it was on June 3 that I learned the next day would be my final
radiation treatment. While my calculations were wrong, I was not
about to dispute the hospital, this time anyway.
So, on June 4, we set out for the last treatment then gathered the
staff to ring the bell. My wife, Vida, wore nice black slacks with a
dressy blouse. We were ready for this wonderful event to take place.
This day was historic in my journey and I felt I had earned every bit
of it and so did Vida.
After the treatment, and after the CLINAC radiation machine
powered down, the
 |
| Vida visiting me in the hospital |
staff came in to release me from the table. I was
excited and they were excited right along with me. I was asked if I
wanted to keep the mask but I had already made arrangements to take
it home with me.
I was putting my shirt back on and asked where the bell was so we
could take some pictures. They looked at each other and said they had
heard that some hospitals have a bell-ringing ceremony, Florida
Hospital Altamonte did not. The bell-ringing following the final radiation treatment is a ritual at some hospitals and radiation treatment centers use the celebrate the final day. It truly is a monumental event for those who have ever been 'exposed' to it.
But, since my hospital did not participate in this program, we created our own celebration at home. It was just as rewarding if not, more so, than the celebration at the hospital may have been.